Parasite Name: Enterobius vermicularis (formerly Oxyuris vermicularis ) Synonyms: pinworm, threadworm, seatworm Classification: Helminth (nematode) Taxonomy: Animalia Nematoda Secernetea Rhabditida Oxyuridae Enterobius vermicularis
Epidemiology
Reservoir
Humans are the only natural host of pinworms, and there currently is no confirmed pinworm reservoir.
Transmission
Life Cycle
Clinical Presentation
Pinworm infection is usually benign, and 1/3 of those infected are asymptomatic.
By far the most common clinical sign of pinworm infection is perianal or perineal itching, and the itching is usually the most severe at night. This is caused by the migration of female pinworms to the anus to lay eggs (specifically, insertion of the tail pin into the mucosa for ovideposition), and scratching leads to finger contamination and subsequently the spread of ovum to others. The scratching may also excoriate the skin and lead to secondary bacterial infections.
Secondary symptoms, which are due to disturbed sleep caused by pruritis, include anorexia and irritability.
However, pinworm infection is not always harmless, as it has been implicated in causing appendicitis (as high as 2.39% of cases in developing countries), intestinal obstruction, intestinal perforation, enterocolitis mimicking Crohn’s disease, and eosinophilic ileocolitis.
Extra-intestinal infections are also possible, and while most involve the female genital tract, infection of other sites has been documented, including the lungs, breast, liver, and spleen.
These extra-intestinal infections may lead to pruritis vulvae, urinary tract infections, postmenopausal bleeding, epididymitis, pelvic mass, chronic sialoadenitis, and unilateral salpingitis, among others. The dead parasites and eggs deposited in ectopic sites can also be responsible for the formation of granulomas and abscesses.
The causative agent :
The adult female has a sharply pointed posterior end, is 8 to 13 millimeters long, and 0.5 millimeter thick.
The adult male is considerably smaller, measuring 2 to 5 millimeters long and 0.2 millimeter thick, and has a curved posterior end.
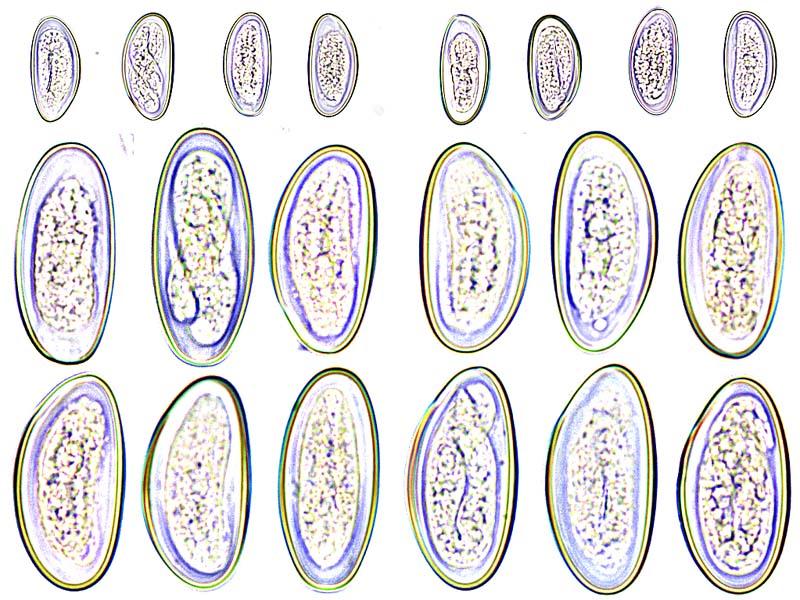
The eggs are translucent and have a surface that adheres to environmental objects.The eggs measure 50 to 60 micrometers by 20 to 30 micrometers, and have a thick shell that is flattened on one side.
The small size and colourlessness of the eggs make them invisible to the naked eye, except in barely visible clumps of thousands of eggs.
Eggs may contain a developing embryo or a fully developed pinworm larva.The larvae grow to 140–150 micrometers in length.
Diagnostic Tests :
The most common means of diagnosing pinworm infection is via the “Scotch tape” test, where a clear adhesive cellulose tape is applied to the anal area early in the morning before bathing or defecation.
This is then observed under a microscope for the presence of pinworm eggs. These eggs may also be stained blue with lactophenol cotton blue, which aids in detection and identification. The sensitivity of this test when performed for three consecutive mornings is 90%. Anal swabs (“Swube tubes:” paddles coated with adhesive material) may also be used.
Therapy
For typical pinworm infections, mebendazole can be used. This is given in single doses of 100 mg by mouth, repeated for two weeks to prevent reinfection, and is arguably the safest and most efficient therapy.
Albendazole may also be used in 100 mg doses for patients under two years old, or in doses of 400 mg for older patients. As in mebendazole, this should also be repeated for two weeks.
References :
http://www.stanford.edu